Abstract
The Role of Blood Cellular Indices in Diabetic Pulmonary Embolism Patients in Predicting Adverse Outcomes.
Bulent Kantarcioglu, Jacob Pozin, Alexander O'Hara, Roumika Patil, Maddie Allen, Emily Krupa, Fakiha Siddiqui, Debra Hoppensteadt, Atul Laddu, Amir Darki, Jawed Fareed.
Introduction: Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is the third leading cause of cardiovascular death. Many established clinical VTE risk factors likely cause thrombosis through the inflammatory pathways. Diabetes mellitus (DM), is an established risk factor for acute myocardial infarction, stroke and peripheral artery disease. On the other hand, its role as an independent risk factor for venous thromboembolism (VTE) is not clearly established. HbA1c is a simple blood test that measures the average blood glucose levels over the past 3 months. It is used as an indicator of glycemic control in DM patients. Complete blood count with differential testing is a cheap and routinely ordered lab test used throughout the clinical course of the patients. Several studies have shown that the increased thrombo-inflammatory response is associated with the changes in blood cellular indices in VTE patients. In this study we sought to determine the relationship between glycemic and blood cellular indices in diabetic PE patients.
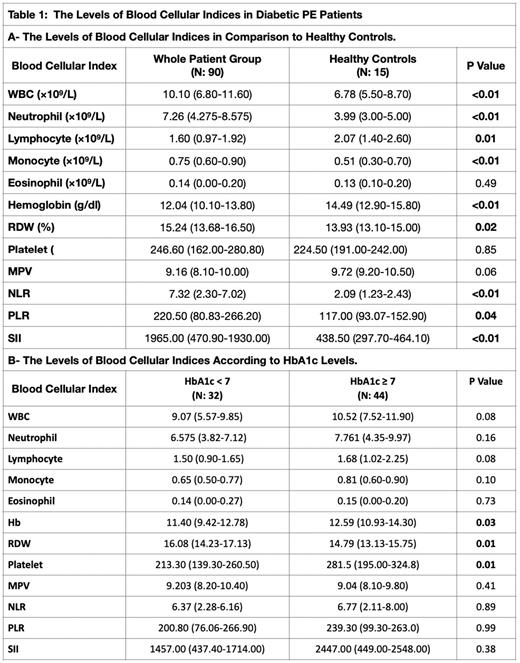
Materials & Methods: The clinical information of 113 diabetic PE patients, including the HbA1c levels within 3 months of PE diagnosis and blood cellular indices were collected through chart review of the electronically medical records of the patients. After exclusion of patients with active cancer, blood cellular indices of diabetic PE patients (n:90) were compared to healthy controls (n: 15) and according to HbA1c levels (n: 76). Statistical difference between PE groups and normal controls were evaluated utilizing nonparametric Mann-Whitney U tests. P < .05 was considered statistically significant.
Results: We did not observe any significant difference in the levels of platelet counts, mean platelet volumes (MPV) and eosinophil counts of the diabetic PE patients in comparison to healthy controls (p > 0.05) (Table 1). The level of white blood cell (WBC), neutrophil, lymphocyte, monocyte, hemoglobin (Hb), red cell distribution width (RDW), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte-ratio (PLR) and systemic immune-inflammation index (SII) counts of the diabetic PE patients were significantly different in comparison to healthy controls (p < 0.05). The patients with poor glycemic control (HbA1c ≥ 7) had significantly higher Hb (p: 0.03) and platelet (p: 0.01) counts and lower RDW values (p: 0.01).
Conclusion: In this study, blood cellular indices were significantly altered in diabetic PE patients in comparison to healthy controls and according to HbA1c levels. This suggests that the blood cellular indices can be a reliable predictor for adverse outcomes in diabetic PE patients. Furthermore, the red blood cell and platelet indices can also be useful predictors for poor glycemic control in diabetic PE patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.